By 1975, the first-ever large-scale, epidemiologic study of the prevalence of AMD was completed, known as the Framingham Eye Study.23 In this particular study of AMD and diet, in order to meet diagnostic criteria for AMD, subjects had to have vision loss to 20/30 or worse as well as drusen — the yellow-white metabolic deposits that we see in the macula of those with AMD, and which are so characteristic of the disease. In the Framingham study, 8.8% of those subjects between 52 and 85 years of age were determined to have AMD, with 27.9% of those between 75 and 85 meeting the definition of disease.
This historical review and recent research indicate that AMD was a medical rarity between 1851 and 1930 and subsequently rose to epidemic proportions in the U.S. by 1975. Perhaps even more concerning is that most developed nations have followed suit, developing high degrees of both incidence and prevalence of AMD in more recent decades. The question is: Why?
The ‘Displacing Foods of Modern Commerce’ – Historical View of AMD and Diet
Until 1880, it was nearly impossible to consume a nutrient-deficient diet, assuming one had enough food and a variety of food. History is very clear that all of the chronic metabolic diseases, i.e., “Westernized” diseases, such as heart disease, cancer, type 2 diabetes, and obesity, all of which are so prevalent today, were medical rarities at the turn of the 20th century.24 Without question, there have always been some people whose nutrition has been poor, sometimes despite a near abundance of nutritious, natural food being available. This was likely the result of being poor, making poor food choices, war or confinement, drought, or perhaps, even conditions associated with poor food choices, such as alcoholism.
In 1880, however, for the first time, refined white wheat flour was produced on a large-scale.
It was 1880 when roller-mill technology replaced stone-mill technology for grinding wheat into flour. Roller-mill technology could entirely remove the bran and the germ of the grain, thereby leaving behind only the endosperm. This type of flour, which was deemed highly desirable at the time, is referred to as “refined” because the roller-mill extraction may also remove the associated B vitamins, E vitamins, omega-3 and omega-6 fats, fiber, and minerals that are naturally found in wheat.25 This was, chronologically, our second major refined, nutrient-deficient food, with refined sugar having been the first. Today, wheat accounts for 20% of the world’s diet.26 By 2005, Loren Cordain, S. Boyd Eaton and colleagues found that 85.3% of the cereal grains consumed in the U.S., particularly including wheat, are now “highly processed refined grains.”27
Introduced just after the American Civil War in the U.S., in 1866, were the seed oils – generally referred to today as “vegetable oils.” The first of these was cottonseed oil.28 This was soon followed by the hydrogenation and partial hydrogenation of cottonseed oil, producing the first-ever artificially created trans-fat. The latter was introduced by Proctor & Gamble in 1911 under the name “Crisco,” which was marketed as “the healthier alternative to lard… and more economical than butter.”29 This first commercially produced trans-fat, i.e., Crisco, remains on the market today.
The so-called “vegetable oils,” along with Crisco, would gradually supplant animal fats, such as butter, lard, and beef tallow. In fact, this was the manufacturer’s intent, i.e., to undersell the more expensive animal fats that had traditionally been used in cooking.
Loren Cordain and colleagues showed that in 1900, the consumption of olive oil, essentially the only edible oil available at that time for most people, would have been in the range of 0.5 pounds per person per year.27 By 2005, however, the average American was consuming 86 pounds of added fats and oils per year, nearly 86% of which was vegetable oils and related products (shortening, margarine, cooking oils, etc.).30 The remaining 14% came from butter, lard, and edible tallow. That is, in the year 1900, 99% of the added fats in cooking would have come from animal fats such as butter, lard, and beef tallow, whereas by 2005, that number had dropped to a mere 14%.
Sugar, our fourth and final major nutrient-deficient processed-food ingredient, had ever-increasing consumption from the 17th century until 1999, after which consumption decreased slightly. Following his historical research of sugar consumption, obesity researcher Stephan Guyenet, Ph.D., wrote:
Wrap your brain around this: in 1822, we ate the amount of added sugar in one 12-ounce can of soda every five days, while today we eat that much sugar every seven hours.31
He found that we consumed 6.2 pounds of sugar per person per year in 1822, which rose to a high of 107.7 pounds per person per year by 1999. This is a 17-fold increase in the consumption of sugar during that period of time.31 In 1999, this amounted to an average consumption of 32 teaspoons per person per day.32
By 2009, 63% of U.S. food consumption was made up of processed, nutrient-deficient, potentially toxic foods, that is, consisting of refined grains (mostly refined wheat flour), vegetable oils, trans-fats, and sugar.33 This is a recipe for metabolic disaster – the same recipe that has led to an epidemic of heart disease, cancer, metabolic syndrome, type 2 diabetes, hypertension, and in my opinion, AMD.
Synthetic Vitamins – Will They Rescue Patients From AMD?
More often than not, synthetic vitamins, i.e., those that come in pills, potions, bottles, and “fortified” foods, fail to deliver beneficial outcomes or their intended results. The fundamental scientific literature is riddled with failures in this regard, as evidenced by recent lectures on this subject by Howard Sesso, Sc.D., MPH, at the Harvard School of Public Health,34 and Jeffrey Tice, M.D., at the University of California San Francisco, Department of Medicine.35
But would synthetic vitamins, which I differentiate from those found in whole foods, be any different in preventing or treating AMD? With regard to the prevention of AMD, the Cochrane Collaboration evaluated four randomized controlled trials that included some 62,520 people. The results? In their words, “People who took these supplements were not at decreased (or increased) risk of developing AMD.” Their final conclusion:
There is accumulating evidence that taking vitamin E or beta-carotene supplements will not prevent or delay the onset of AMD. There is no evidence with respect to other antioxidant supplements, such as vitamin C, lutein, zeaxanthin, or any of the commonly marketed multivitamin combinations.36
Next question: Do synthetic vitamin/multivitamin supplements help delay the progression of AMD that is already established? Utilizing the fair and unbiased results of the Cochrane Collaboration once again, Cochrane found that there were 13 randomized controlled trials that attempted to answer this question. Of those thirteen, twelve showed no benefit. The Cochrane study reported, “The review of trials found that supplementation with antioxidants and zinc may be of modest benefit in people with AMD. This was mainly seen in one large trial {AREDS} that followed up participants for an average of six years. The other smaller trials with shorter follow-up do not provide evidence of any benefit. Although generally regarded as safe, vitamin supplements may have harmful effects.”37
The one trial where synthetic vitamins showed a benefit, the Age-Related Eye Disease Study (AREDS, or “AREDS 1 Trial”), published in 2001, evaluated some 3640 subjects, 55 to 80 years of age, who consumed either a combination of vitamins E and C, beta-carotene, zinc, and copper, or a placebo. For those in AMD categories 3 or 4, which is moderately advanced AMD in both eyes or advanced AMD in one eye, respectively, the results are reported as follows: “The risk reduction for those taking antioxidants plus zinc was 25%.”38
But, the approximate “25% reduction in AMD progression” is a relative number, not absolute. What we want to know is what is our absolute risk reduction because that is what is meaningful if we have AMD. So, let’s examine this further.
For those with category 3 or 4 macular disease, at 5 years from the onset of the study, the probability of progression to advanced AMD was 28% for those given placebo, 23% for those given antioxidants (vitamins E, C, and beta-carotene), 22% for those given zinc, and 20% for those given antioxidants and zinc (the AREDS formula).
From this, the difference between 20% and 28%, is just 8%. Eight percent is the absolute difference in numbers of patients progressing from intermediate AMD in both eyes or advanced AMD in one eye, to advanced AMD, during the five-year follow-up. Eight percent of patients translates to 1 in 12.5, but since you cannot have half a person, this is actually one in 13.
That is, one in 13 was better, as a result of the AREDS formula.
From this, we get the Number Needed to Treat (NNT), which is also 13. That is, you will need to treat 13 patients with the AREDS formula for five years, for one patient to benefit. In the pharmacist’s National PBM Drug Monograph for Ocuvite Preservision, the NNT is reported as 12, but we’re splitting hairs here. They round down since 1 in 12 sounds better than one in 13. Nevertheless, this is still a statement that 12 subjects would have to be treated with the AREDS formula over a period of 5 years for one to benefit, and this was the best-case scenario. That is, 8% of subjects benefitted from taking the AREDS supplement for 5 years.
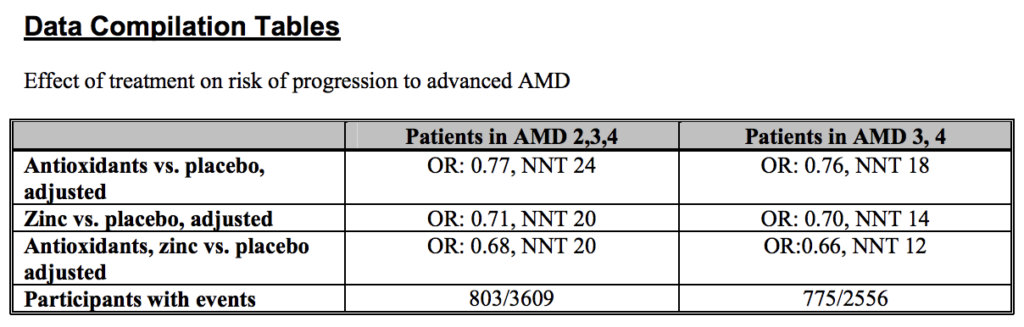
In patients with AMD categories 2, 3, or 4, which is much closer to considering all of those with AMD, the NNT was 20 for those taking the AREDS formula versus placebo. In this scenario, 20 subjects would need to take the AREDS formula for 5 years, for one to benefit. In this case, only 5% of subjects benefitted by taking the AREDS formula for 5 years. Here is the table from the National PBM Drug Monograph:
Click here for the source file for the above data compilation table to download the PDF.
___
Chris A. Knobbe, M.D., is an ophthalmologist and Associate Clinical Professor Emeritus, University of Texas Southwestern Medical Center, in Dallas, Texas, as well as the Founder and President of Cure AMD Foundation™. Dr. Knobbe is author of the book, Ancestral Dietary Strategy to Prevent & Treat Macular Degeneration, which is available at this link.
Dr. Knobbe may be reached directly via the contact form at CureAMD.org.
See references here.