So what’s wrong with the AREDS trial and with Carl Awh’s research? Well, I’m so glad you asked! Finally, we get to the problems with these studies – and what I’ve been itching to tell you all along. The primary problem with the AREDS studies and all related investigations is that diet was never part of the analysis.
It’s worth repeating:
Diet Was Never Part of The Analysis
This is so extraordinarily important that I’d like to repeat the above message three more times in a row. But, I’ll spare you.
The AREDS investigators – as well as all the researchers who followed with additional analyses and re-analyses, at best –may have barely mentioned that diet might play any role in AMD development or progression.
And, ironically, the treatment that was given to the AREDS participants, i.e., at least those in the experimental (non-placebo) groups, is intended to be a little fragment of a healthy diet. The reality is that, as we’ve reviewed, multivitamin/mineral formulas cause us to be a little less healthy and result in our earlier demise, at least on the whole.
And what is the secondary problem, you ask? Well, this is not an issue with the AREDS studies themselves, or with the re-analyses, but rather with almost every single study related to macular degeneration thus far.
More than 99.9% of the available studies do not look at entire diets in relation to AMD prevalence.
Let’s use an analogy. If you’re trying to determine the cause of lung cancer and you have no idea what the cause is, wouldn’t you want to study both populations that have the disease as well as those that don’t?
If 10% of the population you’re studying has lung cancer and they all consume essentially the same diet, and 75% of them smoke, hypothetically, wouldn’t you be interested in comparing a population where 0.1% of the population had lung cancer, regardless of what else you knew about them?
Wouldn’t the latter population with a 0.1% prevalence of lung cancer, perhaps tell you something about the cause of the dreaded disease? And wouldn’t it make sense to compare this population, in great detail, to the population that had the 10% prevalence of lung cancer, which is 100-fold greater?
This is exactly the scenario that I’m referring to with our treatment of macular degeneration, which is based on the AREDS formula and associated studies. In general, almost no one has dared to ask the following question:
“In what populations is macular degeneration a medical rarity, and what are they doing differently? What are they eating?
These are exactly the questions I asked myself back in 2014.
Undoubtedly, in the late 1920s, Weston A. Price, whom I referred to earlier, asked himself similar questions. Although his interest was in dental decay and general physical degeneration, he set out to determine what was different about the diets of people who did not develop those conditions.
Price knew that, even in the 1920s, he could not find an appropriate “control group” in the United States, i.e., people who were not consuming the “experimental diet” (Westernized, man-made, nutrient-deficient, and even toxic foods). Even by the 1920s, people in the United States were already consuming substantial amounts of refined white flour, sugar, canned goods, sweets, vegetable oils, and trans fats. I’ve reviewed this extensively in my book, briefly in the Introduction article on this site, and briefly in most of my live presentations.
Instead of spending decades and millions of dollars studying dental decay and general physical degenerative diseases, such as heart disease, cancer, arthritis, etc., in those people who were already severely afflicted, which is what almost all current studies have done, Price set out to study populations all around the world who did not have these diseases.
The end results, of course, were astonishing. Price discovered that numerous degenerative diseases followed the introduction of Westernized, processed, nutrient-deficient dietary components in significant quantities.
He found, on the contrary, that those who continued to consume their native, traditional, nutrient-dense diets, remained in brilliant health and without degenerative conditions.
Let me remind you: Age-related Macular Degeneration, as its name implies, is a degenerative disease.
For those not aware, in 2013, I hypothesized the following: “The ‘displacing foods of modern commerce’ is the primary and proximate cause of age-related macular degeneration.” We’ve researched this hypothesis, through correlative data, assessing the consumption of the ‘displacing foods’ versus AMD prevalence in 25 nations. This data strongly supports the hypothesis that the ‘displacing foods of modern commerce,’ are indeed the cause of AMD.
Next, we’ll look at just a couple of the 25 nations where we ran these correlative studies.
Where Macular Degeneration is Rarely Found
In an attempt to follow in Weston Price’s footsteps, in early 2015, I set out to try to determine if macular degeneration was confirmed to be rare in any region anywhere in the world. What I found was that, in almost all populations where macular degeneration prevalence had been formally assessed by scientific analysis, the prevalence in recent decades was generally found to be high – often between 20% and about 40%, for those above age 75 to 80. But, let me cite a couple of formal studies to keep this scientific.
Globally, for people between the ages of 45 and 85 years of age, 8.69% have some degree of AMD.72 In the U.S. Beaver Dam Eye Study, conducted between 1988 to 2005 and ongoing, for those aged 43 to 54, AMD affected 8.4%, ages 55 to 64, 13.8% were affected, ages 65 to 74, 18.0% affected, and for those 75 and older, a whopping 29.7% were affected with AMD.73
Without getting into the nitty-gritty detail, in late 2015 and early 2016, I made contact with ophthalmologists in some of the Pacific Island nations. In great contrast to the epidemics of AMD in virtually every developed nation where formal AMD studies have been completed, the prevalence of macular degeneration in the Pacific Island nations of Samoa, Solomon Islands, and Kiribati, is approximately 0.2%, and perhaps even less. This prevalence holds true for people over the age of 60 and into the elderly years.
This is an astonishingly low prevalence of AMD.
This low prevalence is confirmed by chart reviews via the ophthalmologists of these three nations. In fact, in comparing the prevalence of AMD for the approximate same age categories between nations, the U.S. has an approximately 74-fold greater prevalence of AMD if compared to Samoa, Solomon Islands, and Kiribati.
Below is our graph for the Solomon Islands, with the proxy-processed food markers of sugar and vegetable oils, plotted against AMD prevalence.
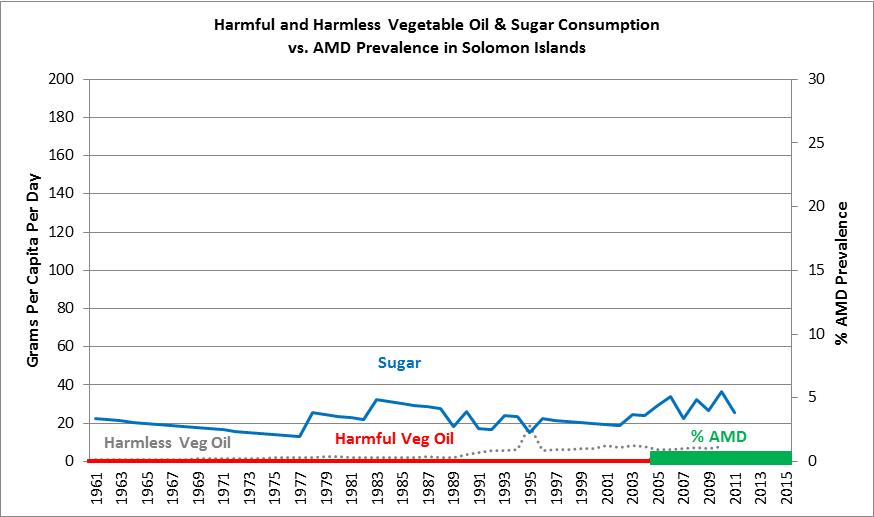
Once we analyzed the diets of these nations, it was clear that this is almost precisely what the hypothesis would have predicted, with the exception of a surprising finding in Kiribati. The consumption of sugar, a proxy marker for processed food, was extremely low in the Solomon Islands, moderately low in Samoa, and moderately high in Kiribati. However, the polyunsaturated (“harmful”) vegetable oil consumption, which is also a strong proxy marker of processed food consumption, was essentially zero in all three nations, since 1961, as evidenced by data from the Food and Agriculture Organization of the United Nations (FAO).74
In general, these are some of the few populations on the planet that have been consuming largely native, traditional diets over a significant part of the past 60 years. This is evidenced by the fact that the majority of the Pacific Island Nations and Territories (PICTs) have relied almost entirely on fish and seafood for their protein sources, along with a quite large variety of roots and tubers, i.e., complex carbohydrates.75 Traditionally, the roots and tubers consumed by Pacific Islanders have included taro, sweet potatoes, and yams, and they’ve also traditionally consumed a large variety of tropical fruits that were eaten in large quantities, including bananas, plantains, mangoes, papayas, and pineapples.76
The coconut is a major subsistence crop in the Pacific Island nations, where every edible part of the coconut is eaten, including a substantial reliance on coconut milk and coconut oil.77
Hughes and Lawrence of the University of Queensland, Brisbane, Australia, have shown that many of the PICTs have experienced Westernization of the diet in more recent decades, as evidenced by increasing reliance and consumption of commercialized, nutrient-deficient, imported foods.78 These foods are primarily being imported from Australia, New Zealand, and the USA, all of which have been accused of food “dumping,” with allegations relating to poor nutrition quality. This, of course, has been followed by a severe overall decline in the health of Pacific Islanders, with dramatically increasing rates of obesity, communicable, and non-communicable diseases.78
In the island nations of Solomon Islands, Samoa, and Kiribati, however, the transition to Westernized diets has obviously not occurred to the extent that it has in many other Pacific Islanders (their sugar and vegetable oil consumption data confirm by FAO) and, as such, they’ve not succumbed to many of the chronic, degenerative diseases that take at least a few decades to develop, such as heart disease and macular degeneration.
“The fate of nations is determined by what they eat. (Jean Anthelme Brillat-Savarin, 1825)
When the prevalence of AMD was once found to be low in various populations, such as the Japanese people (of Japan), the assertion was made that the Japanese were “genetically protected.” In fact, I recall this assertion in regards to the Japanese (again, of Japan) when I was a resident in ophthalmology at the University of Colorado Health Sciences Center, in Denver, in the years 1991 to 1994.
This assertion, i.e., that races and cultures are “genetically protected,” is what those of us in ancestral nutrition now refer to as “playing the genetics card.” This, of course, is the incorrect and inchoate belief system that people are protected from degenerative diseases based purely on their genetic constitution. No doubt, we all have genetic predispositions, but Price’s treatise on this subject, Nutrition and Physical Degeneration, left no doubt that not a single racial or cultural group can retain immunity to the ravages of nutrient-deficient, processed food-laden diets. People of every race, ethnicity, or cultural heritage are at risk – and of course – this is only logical.
Why should we expect that anyone, of any given race, should be immune to the ravages of nutrient-deficient diets, replete with toxic components?
With regard to AMD prevalence in Japan, between the years 1974 and 1979, at the Nagoya University Hospital, in Nagoya, Japan, only 24 eyes with dry macular degeneration and 36 eyes with wet macular degeneration were found among 31,334 outpatient visits during that period. By estimating that 90% of those seeking eyecare were over age 40, which is quite typical (remember, these are people visiting a hospital for eyecare, not an outpatient optometry clinic), this leaves 60 patients affected by AMD, out of some 28,201 total patient visits, for an approximate prevalence of 0.2%. This assumes only one patient represents each eye affected, which is highly unlikely and would, therefore, make the prevalence of AMD during that period potentially even lower.
Less than 30 years later, in 2007, the Hisayama Study in Japan found that, of residents age 50 and above, 10.0% had early AMD and 1.4% had late AMD, for a total AMD prevalence of 11.4%.79
And, just in case we might think that the Hisayama Study was a fluke, an unusual population, or in any other way non-representative of rising AMD prevalence in Japan, in 2013, the Nagahama Study in Japan found early AMD prevalence of 16.1% in the 50 to 59 year-old category, and 31.2% in the 70 to 74-year-old category.80 In this same study, advanced AMD was present in 0.27% of the 50 to 59-year-olds and 0.98% of the 70 to 74-year-olds.
If we only compare the prevalence of AMD in the late 1970s to that of the 2007 Hisayama study in Japan, this is a staggering 57-fold increase in the prevalence of AMD in a span of just 30 years.
This cannot possibly be explained by genetics – or the aging of a population.
There are multiple other large population examples of the AMD prevalence most definitely rising in such time periods, which I’ve reviewed (once again) in the Introduction, and in my book.
The question is – what could possibly induce a 57-fold increase in the prevalence of AMD in Japan in just 30 years?
The answer, of course, is Westernization of the diet.
And we have the data to prove it – see the graph below:
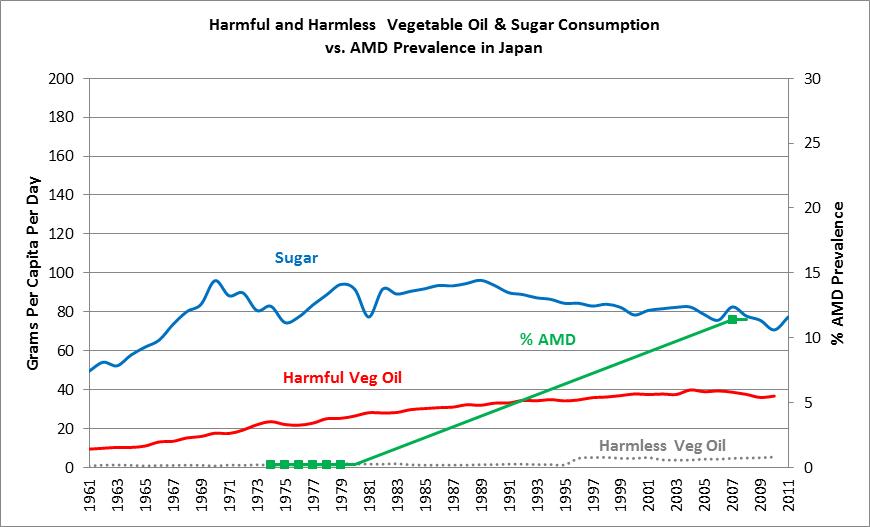
Once again, if we examine sugar consumption, a well-known proxy-marker of processed food consumption, we see that consumption in Japan in 1961 was roughly 50 grams per day, and subsequently rose to 80 to 90 grams per day in succeeding decades. The “harmful vegetable oils,” which are those containing significant polyunsaturated oils, rose from 9 grams per day in 1961, to 40 grams per day by 2003, which is a 4.5-fold increase in the consumption of these dangerous vegetable oils. This, of course, indicates a dramatic increase in the consumption of Westernized, processed, nutrient-deficient foods, in this short period of time.
_____________
This is Part Six of an eight-part series.
________________________
Part 1: Are the Best Vitamins for Macular Degeneration Synthetic?
Part 2: The History of Vitamins
Part 3: Vitamins and AMD
Part 4: Vitamins, AMD, and The Effects of Supplementation
Part 5: Vitamin Studies for AMD (AERDS)
Part 7: Coming soon
Part 8: Coming soon

