This piece will review the signs, symptoms, and diagnosis of Age-related Macular Degeneration (AMD) both wet and dry – the number one cause of blindness in people over 65. Much like that of literally thousands of websites, it is purely for the sake of completeness and for those who want to understand what and where the macula is as well as the basics of dry and wet AMD. This page will not cover risk factors for AMD, exactly what occurs at the molecular (microscopic) level to produce AMD, nor will it cover prevention or treatment for AMD. For those who want to understand the basics of the hypothesis and supportive research which we have completed regarding how Westernized diets lead to AMD — and what you can do about it — go to this “Introduction.” Or if you desire to know all the nitty-gritty details, including an extensive review of the history of AMD, the big-picture on diets and macular degeneration, and the ‘whole kahuna’ on ancestral dietary management, consider my book, Ancestral Dietary Strategy to Prevent and Treat Macular Degeneration.
Age-related Macular Degeneration – AMD
Age-related macular degeneration, also known as AMD or ARMD, is the leading cause of irreversible vision loss and blindness in Americans who are age 65 and older. This disease affects about 10 to 15% of Americans between the ages of 65 and 75 and is present to some degree in about 30% of the population that is 80 years of age and older.
Macular degeneration, or AMD, is a disease of the macula. The macula is the central retina, which is really the part of the eye that is analogous to the film of a camera (think image sensor in today’s digital cameras). The macula of the eye only accounts for the central 10 degrees of vision, approximately, but this ten degrees is by far the most important part of your vision. When you look at anything, what you’re really most interested in is what your macula sees. Your macula would see, for example, someone’s face, the words you’re reading, or the road ahead as you drive.
If the macula degenerates, so does your central vision. The degree that it degenerates is consistent with the degree that your central vision would be impaired.
Dry AMD and Wet AMD
 There are two basic forms of AMD: “Wet AMD” and “Dry AMD.” Let’s talk about dry AMD first.
There are two basic forms of AMD: “Wet AMD” and “Dry AMD.” Let’s talk about dry AMD first.
The dry form of AMD accounts for around 85 to 90% of patients with the disease. Fortunately, dry AMD generally does not cause as much vision loss. However, dry AMD can progress into “late AMD,” which would include severe geographic atrophy and wet AMD, and this is the usual progression.
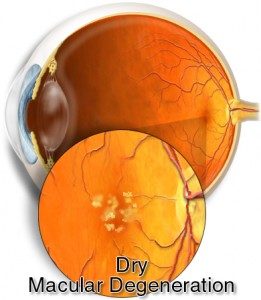
Dry AMD
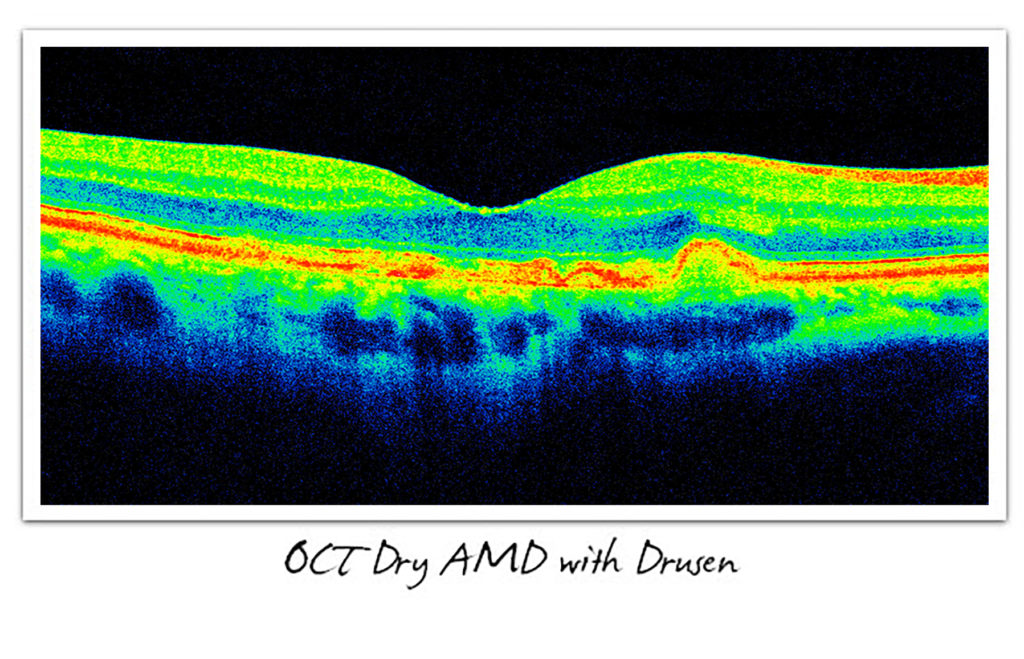
Dry AMD is present when there is retinal pigment epithelium (RPE) atrophy, with associated loss of photoreceptors (rods and cones), and which is also characterized by drusen in the macula. Drusen are small, yellowish “metabolic” deposits that accumulate in the RPE layer of the macula. As the drusen increase in size and number, the severity of the disease usually progresses. Gradual central vision loss typically occurs with dry AMD, but most patients do not have severe visual loss.
As the disease progresses, there is the development of geographic atrophy (GA), which is actually a loss of the retinal photoreceptors (rods and cones) themselves, loss of retinal pigment epithelium (RPE), and an associated thinning of the retina. Geographic atrophy may be associated with severe vision loss.
Wet AMD
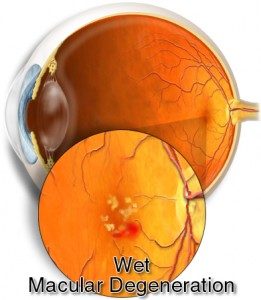 Wet AMD occurs when there is a break in Bruch’s membrane, which is a layer beneath the retina, and abnormal vessels from below push through that compromised layer and begin to grow and leak blood or fluid into the retina itself. The bleeding and/or fluid in the retina damages the photoreceptors themselves, which ultimately may be destroyed, resulting in permanent and irreversible blind spots.
Wet AMD occurs when there is a break in Bruch’s membrane, which is a layer beneath the retina, and abnormal vessels from below push through that compromised layer and begin to grow and leak blood or fluid into the retina itself. The bleeding and/or fluid in the retina damages the photoreceptors themselves, which ultimately may be destroyed, resulting in permanent and irreversible blind spots.
This process of new vessel growth beneath the retina proper, known as choroidal neovascularization (CNV), may be associated with a severe and potentially permanent distortion of the retinal anatomy. Unless this process can be halted and reversed early after the onset of the fluid (and/or blood) leakage, the end result may be severe and permanent, irreversible vision loss.
Signs and Symptoms of AMD
Dry AMD will typically cause a slow, painless loss of central vision. However, there’s really no way for an individual who is losing vision to know if this is due to macular degeneration. Only a trained eye-care practitioner, such as an ophthalmologist (M.D.) or optometrist (O.D.), can determine if AMD exists, via a complete eye exam.
In wet AMD, the affected individual may notice distortion of central vision, known as metamorphopsia. A patient with metamorphopsia complains that lines, which should appear straight, are wavy. This may be noticed by looking at the edge of a door, door jamb, or the straight edge of just about anything else. Eye-care providers use an “instrument” known as an Amsler grid to help detect this condition.
Amsler Grid: The image on the left is the actual image and normally, is perceived as such. The image on the right is asimulation of how the image might be perceived by the affected eye of an individual with wet AMD.
An Amsler grid consists simply of a graph of intersecting lines, with a dot in the center, designed to be the focal point. A patient is asked to look at the grid – and actually “stare” at the central black dot. Then, while staring, they take notice of the rest of the grid. If the normally straight lines on any part of the grid are wavy or distorted, the patient has metamorphopsia. Again, this might be indicative of the development of wet AMD, especially in a patient who has already been diagnosed with dry AMD.
Diagnosis of AMD
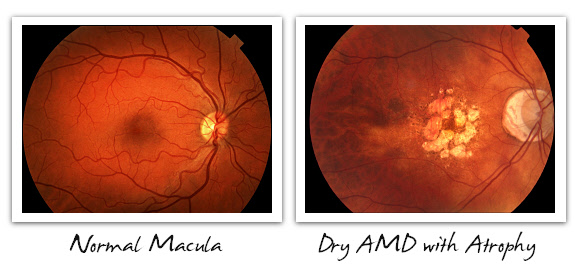
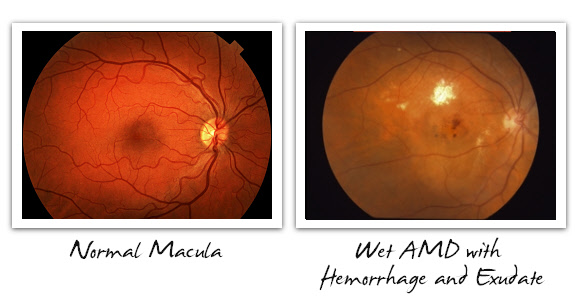
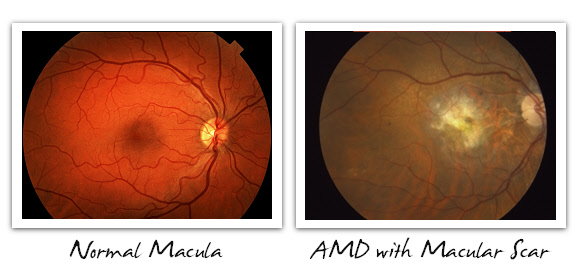
Below, we see what we eyecare providers call fundus images. The fundus includes the retina, optic nerve, vessels, and of course, the macula, which is the central retina. On the left of each pair of images is a normal macula, for reference, while on the right side is dry AMD with drusen, dry AMD with geographic atrophy, and wet AMD with hemorrhage and exudative deposit. These are some typical cases that ophthalmologists and optometrists might see when evaluating patients with AMD. The images themselves are taken with a fundus camera, and the best images are always produced through a dilated pupil.
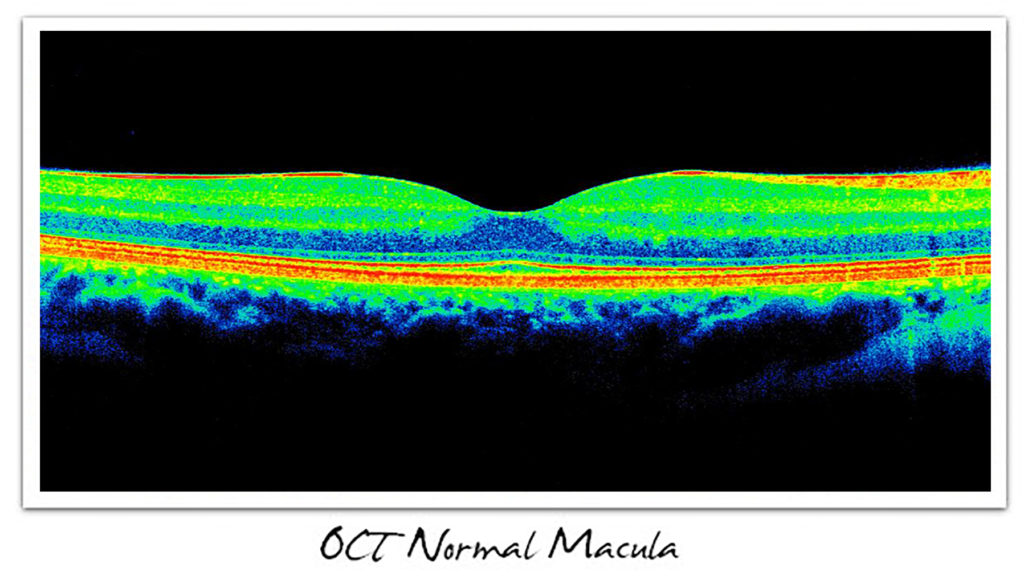
Ocular Coherence Tomography (OCT) Imaging of the Macula
Many eyecare providers routinely screen their patients who are older than approximately 40 or 50 years of age using Ocular Coherence Tomography, better known as OCT.
OCT, scientifically defined, is an interferometric technique, employing near-infrared laser light (i.e., long wavelengths), to capture micrometer resolution, three-dimensional images from within optically scattering media.
OCT is a technique for obtaining sub-surface images of translucent or opaque tissues (think the back of the eye – retina, RPE, and choroid) at a resolution better than 10 micrometers (microns). Prefer the laymen’s terms? OCT is like the ophthalmologist’s MRI — of the eye!
This resolution and imaging of the retina have revolutionized the practice of ophthalmology because it allows eye-care practitioners to see that which could never before have been seen with any type of microscope.
Below is an image of the Zeiss, Cirrus™ HD-OCT, which happens to be one of the most commonly used OCT devices by ophthalmologists, due to its amazing imaging speed and high-resolution.
The OCT literally creates virtual biopsies of the retina, as if you had removed the patient’s eye, had it prepared in a lab, and then sliced up the macula into a thousand, razor-sharp, histologic (tissue) sections, each of which is beautifully stained. But, it’s even better than that because it represents the live, unchanged tissue of the retina. Plus, it uses no ionizing radiation (x-rays), the light is invisible to the patient (making it completely comfortable), and the images can be taken in just a few minutes, even without dilating the pupil.
Fluorescein Angiography (FA) — Imaging in Suspected Wet AMD
When ophthalmologists suspect wet AMD, based either on symptoms such as visual distortion or metamorphopsia (wavy vision), in most cases an OCT image will be obtained first. If it appears that wet AMD may be present, as indicated on the OCT, then a fluorescein angiogram (FA) or indocyanine green (ICG) angiogram may be obtained as well. This helps the ophthalmologist to determine with even greater certainty what the diagnosis actually is because the angiogram will show whether or not the area of concern is actively leaking fluid.
In some cases, the FA is omitted, if the diagnosis appears certain, based on the OCT. Patients should realize that there are numerous conditions that affect the macula, and the results of the imaging procedures will help us ophthalmologists to make a diagnosis, just as an MRI assists in making a diagnosis of innumerable conditions.
Below are images of an FA in both a normal eye and in an eye with wet AMD.
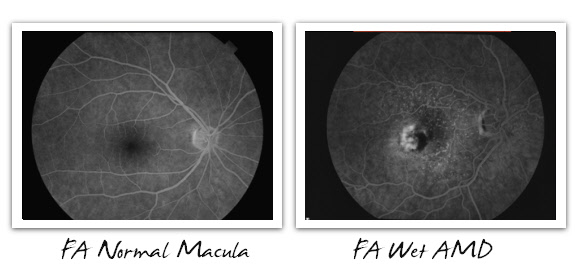
In fluorescein angiography (FA) and indocyanine green angiography (ICG), one of the respective dyes is given to the patient intravenously, usually via a vein in the arm. Then, photos of the back of the eye are taken using a fundus camera.
The illustration above happens to show a Zeiss NM/FA fundus camera, which produces brilliant digital images that can instantly be reviewed on the computer screen, permanently stored in digital media, and printed out in various resolutions as needed.
FA and ICG angiography are both extraordinarily safe procedures – and once the eyes are dilated, the angiography only takes a few minutes to actually complete. The ophthalmologist will then review the images, make correlations with the OCT, and then discuss the findings with the patient.
For patients who have been diagnosed with wet AMD and are being treated, follow-up examinations are usually completed using OCT, and FA’s (angiograms) are utilized when the diagnosis is uncertain based on the OCT.
Summary and Conclusions
Age-related macular degeneration, or AMD, is the leading cause of irreversible vision loss and blindness in developed nations, worldwide. We have reviewed the fundamentals of the signs and symptoms of macular degeneration, along with exactly how eye-care practitioners, i.e., ophthalmologists (Eye M.D.) and optometrists (O.D.), diagnose this disease using patients’ presenting signs and symptoms — as well as fundus evaluation, imaging with fundus photography, OCT imaging, and fluorescein and indocyanine green (ICG) angiography.
____
It is the mission of Cure AMD Foundation™ to prevent vision loss from AMD in millions of people, on a global scale. It is our collective belief that this disease can be prevented through ancestral dietary strategy and sacred foods. Our mission is to be an advocate for this hypothesis and supportive research and to spread this message to ophthalmologists, optometrists, vision scientists, and the public at large. We also intend to conduct and publish additional research in this regard. For those who want a brief summary of the dietary (nutritional) hypothesis and supportive research that we’ve conducted thus far, click the following link to view the Introduction. And for those who desire to have a deep understanding of this hypothesis, supportive research, and dietary recommendations, consider my book, Ancestral Dietary Strategy to Prevent and Treat Macular Degeneration.